Responsive Feeding
Overview
As part of the baby friendly initiative, healthcare professionals (HCPs) have a responsibility to support parents and carers to engage in responsive feeding for breastfed and formula-fed infants.1 Responsive feeding has been shown to be protective against obesity in children later in life.2 This article explores overfeeding a baby and its effects, recognising hunger cues and the importance of responsive feeding.
What is overfeeding?
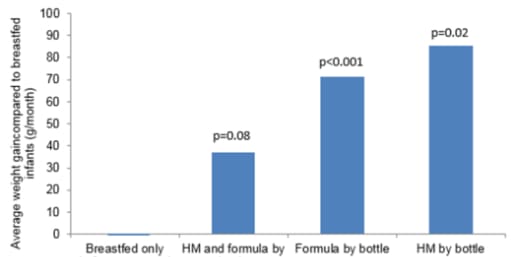
Obesity in children has been attributed to factors that occur during the first 1000 days of life, which spans from conception to 2 years of age. These include, maternal nutrition, genetic predisposition, breastfeeding and introduction to solids.2 Feeding in infancy (<6 months of age) is thought to be a prime time for appetite and satiety regulation as it occurs during a period of biological malleability which can determine long-term eating habits, growth parameters and future metabolic responses.3 It has been shown that breastfed babies self-regulate their intake in a more efficient way than bottle-fed babies.2
It has been suggested that feeding infants on a three hourly schedule instead of when they show hunger cues, may have a role in the development of obesity in later life by impairing an infant’s response to fullness cues.4,5
One randomised clinical trial provided education to parents which included recognising hunger and satiety cues, feeding in response to hunger and not as an emotional response and age-appropriate portion sizes. The study demonstrated that providing parents with responsive feeding support, reduced rapid infant weight gain, reduced prevalence of overweight infants (at age one year) and improved adherence to dietary guidelines post transition to solid food.6 The intervention benefited both breastfed and formula-fed infants.
The importance of responsive feeding
Responsive breastfeeding recognises that feeds do not simply provide nutrition, but also offers love, comfort and reassurance between a mother and her baby.7 Responsive breastfeeding has multiple benefits including satisfying hunger and providing reassurance for a distressed baby. Therefore, breastfeeding may vary in frequency and length, depending on the needs of the mother and baby. Parents should be reassured that breastfed babies cannot be ’overfed’ or ’spoilt’ by frequent breastfeeding.7
It is possible to practice responsive feeding when formula-feeding, however it is important to acknowledge the risks of overfeeding.7 A systematic review found a positive relationship exists between ‘indulgent feeding’ and overweight/obesity in children and infants. A proposed explanation for these associations, particularly during early years, is parents’ use of feeding as a strategy to calm their child’s behaviour.8 Parents should be supported to identify their baby’s hunger and fullness cues and how to effectively feed whilst keeping their babies close to promote bonding.9 The following strategies can help implement responsive feeding in formula-fed infants:7,9
-
Offer the bottle in response to hunger cues.
-
Gently invite the baby to accept the teat.
-
Practice paced bottle feeding.
-
Avoid forcing the baby to finish the feed.
-
Practice bonding with the baby through eye and skin-to-skin contact.
-
In the first few weeks, try to minimise the number of people regularly feeding the baby to help strengthen the bond between baby and parent.
Responsive feeding helps to promote attentiveness to internal cues of hunger and satiety and successful progression to independent feeding throughout childhood.10
Importance of recognising hunger and fullness cues for responsive feeding
There still remains the common belief amongst HCPs that a ‘normal’ feeding pattern is to feed every three hours. However, to effectively practice responsive feeding, it is important that parents are taught how to recognise the signs babies use to communicate their hunger and fullness. This is particularly important in formula-fed babies to help prevent overfeeding. The video clips below are useful tools to help support parents tune into their baby’s own cues.
Parents of formula-fed babies should be reassured that there are other effective methods to calm and soothe babies in the absence of breastfeeding (e.g., cuddling and skin-to-skin contact) which will continue to strengthen the parent-infant attachment.7
Summary
When supporting parents with infant feeding, HCPs should engage in respectful discussions with regard to feeding. Clinical evidence supports the practice of responsive feeding in both breastfed and formula-fed infants.
Related articles
-
UNICEF. Baby Friendly Standards - Baby Friendly Initiative. [Internet]. 2014. [cited August 2022]. Available from: https://www.unicef.org.uk/babyfriendly/about/standards/
-
Ramirez-Silva I, et al. 2021. Infant feeding, appetite and satiety regulation, and adiposity during infancy: a study design and protocol of the 'MAS-Lactancia' birth cohort. BMJ Open;11(10):e051400. doi: 10.1136/bmjopen-2021-051400.
-
Disantis KI, et al. 2011. Do infants fed directly from the breast have improved appetite regulation and slower growth during early childhood compared with infants fed from a bottle? Int J Behav Nutr Phys Act;8:89. Doi: 10.1186/1479-5868-8-8
-
Watchmaker B, et al. 2020. Newborn feeding recommendations and practices increase the risk of development of overweight and obesity. BMC Pediatr;20(1):1-6.
-
Disantis K, et al. 2011. The role of responsive feeding in overweight during infancy and toddlerhood: a systematic review. Int J Obes (Lond);35(4):480
-
Paul I, et al. 2018. Effect of a Responsive Parenting Educational Intervention on Childhood Weight Outcomes at 3 Years of Age: The INSIGHT Randomized Clinical Trial. JAMA;320(5):461
-
UNICEF. Responsive feeding: supporting close and loving relationships. [Internet]. 2016. [cited August 2022]. Available from: https://www.unicef.org.uk/babyfriendly/wp-content/uploads/sites/2/2017/12/Responsive-Feeding-Infosheet-Unicef-UK-Baby-Friendly-Initiative.pdf
-
Hurley K, et al. 2011. A systematic review of responsive feeding and child obesity in high-income countries. J Nutr;141(3):495-501.
-
National Institute for Health and Care Excellence (NICE). Postnatal Care. NG194. [Internet]. 2021. [cited August 2022]. Available from: https://www.nice.org.uk/guidance/ng194/chapter/recommendations#responsive-feeding
-
Black M and Aboud F. 2011. Responsive feeding is embedded in a theoretical framework of responsive parenting. J Nutr;141(3):490-4.
IMPORTANT NOTICE:
We believe that breastfeeding is the ideal nutritional start for babies, and we fully support the World Health Organization’s recommendation of exclusive breastfeeding for the first six months of life followed by the introduction of adequate nutritious complementary foods along with continued breastfeeding up to two years of age. We also recognise that breastfeeding is not always an option for parents. We recommend that healthcare professionals inform parents about the advantages of breastfeeding. If parents choose not to breastfeed, healthcare professionals should inform parents that such a decision can be difficult to reverse and that the introduction of partial bottle-feeding will reduce the supply of breast milk. Parents should consider the social and financial implications of the use of infant formula. As babies grow at different rates, healthcare professionals should advise on the appropriate time for a baby to begin eating complementary foods. Infant formula and complementary foods should always be prepared, used and stored as instructed on the label in order to avoid risks to a baby’s health.